Tamoxifen and Bone Density⁚ A Comprehensive Guide
This guide explores the complex relationship between tamoxifen, a common breast cancer treatment, and bone density. We’ll examine its effects on bone health in both pre- and postmenopausal women, highlighting the importance of monitoring and strategies for maintaining bone strength during treatment. Understanding these aspects is crucial for optimizing patient care and well-being.
Introduction⁚ Understanding the Impact of Tamoxifen
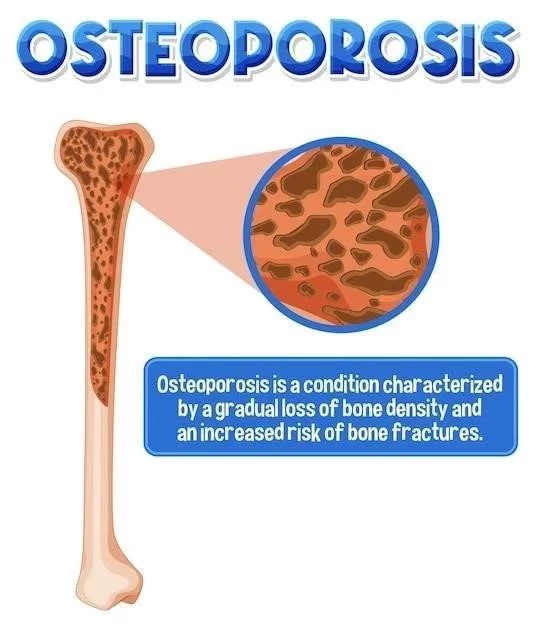
Tamoxifen, a selective estrogen receptor modulator (SERM), is a cornerstone treatment for estrogen receptor-positive breast cancer. While highly effective in combating cancer, its impact on bone density presents a crucial consideration. This is because tamoxifen’s mechanism involves interacting with estrogen receptors, influencing bone metabolism. In postmenopausal women, where estrogen levels are naturally low, tamoxifen can exhibit estrogen-like effects on bones, potentially improving bone density and reducing fracture risk. Studies have shown a modest increase in bone mineral density (BMD) in the lumbar spine in postmenopausal women treated with tamoxifen. However, the effects in premenopausal women are less clear, with some studies suggesting a potential for bone loss, particularly in the initial years of treatment. This nuanced effect necessitates careful monitoring and personalized management strategies for optimal bone health during tamoxifen therapy. Understanding these diverse responses is critical for healthcare professionals and patients alike.
Tamoxifen’s Mechanism of Action and its Estrogen-like Effects on Bones
Tamoxifen’s actions are multifaceted, stemming from its ability to bind to estrogen receptors. In breast tissue, it acts as an antagonist, blocking estrogen’s stimulatory effects on cancer cells. This anti-estrogenic property is the basis of its efficacy in breast cancer treatment. However, in bone tissue, tamoxifen’s behavior is more complex. It acts as a partial agonist, meaning it can stimulate some estrogen receptor activity while also blocking others. This partial agonist activity on bone receptors is responsible for the observed bone-preserving effects in postmenopausal women. In these women, where endogenous estrogen is low, tamoxifen’s partial agonism can help maintain bone mineral density (BMD) and reduce the risk of osteoporosis and fractures. The contrasting effects in premenopausal women, where endogenous estrogen is higher, might be attributed to the overall influence on the estrogen balance, leading to a potential for bone loss in some cases. This dual nature of its interaction with the estrogen receptor system in bones highlights the importance of considering individual patient factors when assessing the impact on bone health.
Bone Density Changes in Postmenopausal Women⁚ A Positive Outlook
Postmenopausal women, already at increased risk for osteoporosis due to declining estrogen levels, often face additional bone health challenges during breast cancer treatment. However, for these women, tamoxifen frequently offers a positive influence on bone density. Its partial estrogen agonist activity helps mitigate the bone loss typically associated with postmenopause. Studies have consistently demonstrated that tamoxifen can lead to a modest increase in bone mineral density (BMD) at the lumbar spine, a key indicator of overall bone health. This bone-preserving effect translates to a reduced risk of fractures, a significant concern in this population. The magnitude of BMD improvement varies among individuals, influenced by factors such as duration of treatment, baseline BMD, and adherence to lifestyle recommendations. While not a guaranteed solution for osteoporosis prevention, tamoxifen’s positive effect on bone density in postmenopausal breast cancer patients provides a valuable therapeutic benefit, supplementing other strategies for maintaining bone health.
The Role of Tamoxifen in Preventing Bone Loss in Postmenopausal Breast Cancer Patients
Postmenopausal breast cancer patients face a double challenge⁚ the risk of bone loss associated with estrogen deficiency and the need for effective cancer treatment. Tamoxifen, in this context, plays a crucial role in mitigating bone loss. By acting as a partial estrogen agonist in bone tissue, it helps counter the negative impact of estrogen depletion on bone health. This protective effect translates to a reduced risk of osteoporotic fractures, a significant concern for this patient population. The beneficial effects on bone density are particularly valuable given the increased longevity achieved through improved cancer treatments. By slowing bone loss, tamoxifen contributes to maintaining overall skeletal health and improving quality of life during and after cancer therapy. However, it’s crucial to remember that tamoxifen is primarily a cancer treatment; its bone-preserving properties are a secondary yet important benefit. Individual responses vary, and regular monitoring of bone density is essential to ensure appropriate management.
Clinical Studies⁚ Evidence Supporting Tamoxifen’s Bone-Preserving Effects
Numerous clinical trials have investigated the effects of tamoxifen on bone mineral density (BMD) in postmenopausal women with breast cancer. These studies, while varying in design and population size, consistently demonstrate a positive impact of tamoxifen on bone health. Many have shown a modest but statistically significant increase in lumbar spine BMD in women receiving tamoxifen compared to control groups. This increase is often observed over several years of treatment, suggesting a sustained bone-preserving effect. While some studies have reported smaller effects or even minor decreases in BMD in certain subgroups, the overall body of evidence strongly supports tamoxifen’s ability to slow bone loss and potentially increase BMD in postmenopausal women with breast cancer. These findings underscore the clinical relevance of considering tamoxifen’s influence on bone health when formulating treatment plans for this patient population. Further research continues to refine our understanding of this complex interplay between cancer treatment and skeletal health.
Dosage and Duration of Tamoxifen Treatment⁚ Optimizing Bone Health
The optimal dosage and duration of tamoxifen therapy for breast cancer are determined primarily by oncologic considerations. However, understanding the impact on bone health is crucial for personalized treatment strategies. While higher doses might offer greater anti-cancer effects, they may not necessarily translate to proportionally increased bone-preserving benefits. In fact, excessively high doses could potentially outweigh the positive effects on bone density. The duration of treatment also plays a role. Longer durations generally lead to more significant improvements in BMD, although this benefit must be balanced against the potential for increased side effects. Therefore, the decision regarding dosage and duration should be a collaborative effort between the oncologist and other healthcare professionals involved in the patient’s care. Regular monitoring of BMD allows for adjustments to the treatment plan, ensuring that the benefits of tamoxifen in combating cancer are maximized while mitigating potential risks to bone health.
Bone Density Changes in Premenopausal Women⁚ A Different Perspective
In premenopausal women, the effects of tamoxifen on bone density differ significantly from those observed in postmenopausal women. While postmenopausal women often experience a positive impact on BMD, premenopausal women may exhibit a different response. This discrepancy arises from the differing hormonal environments. Premenopausal women have higher endogenous estrogen levels, influencing how tamoxifen interacts with estrogen receptors in bone. Some studies suggest that tamoxifen may lead to a slight decrease in BMD, particularly during the initial years of treatment, although this effect is often not clinically significant and may not persist long-term. This potential for bone loss necessitates careful monitoring, especially in premenopausal women undergoing tamoxifen therapy. Individual responses vary widely, highlighting the importance of personalized approaches and close collaboration between healthcare professionals to optimize both cancer treatment and bone health management.
Tamoxifen’s Effect on Premenopausal Women⁚ Potential for Bone Loss
Unlike the generally positive effects seen in postmenopausal women, tamoxifen’s impact on bone density in premenopausal women is more complex and can potentially lead to bone loss. This difference stems from the presence of higher endogenous estrogen levels in premenopausal individuals. Tamoxifen’s interaction with estrogen receptors in bone tissue, while exhibiting partial agonist activity, might disrupt the natural estrogen balance in premenopausal women, potentially leading to reduced bone mineral density (BMD). Studies have indicated a possible small decrease in BMD during the early stages of tamoxifen treatment, although the long-term effects and clinical significance remain areas of ongoing research and debate. This potential for negative bone health consequences emphasizes the importance of careful monitoring of BMD in premenopausal women receiving tamoxifen. Individualized risk assessment and proactive strategies for bone health preservation are essential for this patient group.
Factors Influencing Bone Density Changes During Tamoxifen Therapy
The impact of tamoxifen on bone density is not uniform; several factors influence the individual response. Menopausal status is a primary determinant, with postmenopausal women often experiencing bone-preserving effects while premenopausal women may show a different response. Baseline bone mineral density (BMD) prior to treatment is another crucial factor; individuals with lower baseline BMD may be more susceptible to negative effects. Genetic predisposition, lifestyle choices (diet, exercise, smoking, alcohol consumption), and the presence of other medical conditions also play a significant role. Furthermore, the duration and dosage of tamoxifen therapy influence bone health outcomes. Concomitant medications, particularly those affecting bone metabolism, can also interact with tamoxifen, modifying its overall impact on bone density. Therefore, a comprehensive assessment of these individual factors is crucial for personalized management and proactive strategies to optimize bone health during tamoxifen treatment. Regular monitoring of BMD helps tailor the treatment approach to each patient’s specific needs.
The Importance of Monitoring Bone Density During Tamoxifen Treatment
Regular monitoring of bone density is paramount during tamoxifen therapy to assess its impact on bone health and to identify potential risks early. This proactive approach allows for timely interventions to mitigate any negative effects and optimize overall skeletal health. Baseline bone mineral density (BMD) measurement before starting tamoxifen establishes a reference point for comparison. Subsequent BMD assessments at regular intervals, typically annually or biannually, track changes and allow for early detection of significant bone loss. This monitoring enables healthcare professionals to personalize treatment strategies and adjust the course of therapy if necessary. For example, if significant bone loss is detected, supplemental interventions like calcium and vitamin D supplementation, exercise programs, or even bisphosphonates, might be considered. The frequency and type of monitoring should be tailored to individual risk factors and patient characteristics, emphasizing the importance of a collaborative approach between patient and healthcare provider.
Lifestyle Modifications to Enhance Bone Health During Tamoxifen Therapy
While tamoxifen plays a significant role in breast cancer treatment, lifestyle modifications can complement its effects and further enhance bone health. A balanced diet rich in calcium and vitamin D is crucial for maintaining bone density. Calcium-rich foods like dairy products, leafy greens, and fortified foods should be incorporated into the daily diet. Vitamin D, essential for calcium absorption, can be obtained through sunlight exposure, dietary sources, or supplementation. Regular weight-bearing exercise is another key component. Activities like walking, jogging, dancing, and weight training help stimulate bone formation and improve bone strength. Maintaining a healthy weight reduces stress on bones and minimizes fracture risk. Smoking cessation is vital, as smoking is strongly associated with reduced bone density and increased fracture risk. Limiting alcohol consumption also plays a protective role. These lifestyle changes, integrated into a comprehensive approach to bone health, can synergistically enhance the positive effects of tamoxifen therapy and reduce the risk of osteoporosis.
Nutritional Strategies⁚ Calcium and Vitamin D Intake
Optimal nutrition plays a vital role in supporting bone health, especially during tamoxifen therapy. Calcium is the fundamental building block of bone, and adequate intake is crucial for maintaining bone density. Dietary sources of calcium include dairy products (milk, yogurt, cheese), leafy green vegetables (kale, spinach), and fortified foods (cereals, juices). If dietary intake is insufficient, calcium supplements can be considered, but it’s advisable to consult a healthcare professional before starting supplementation to determine the appropriate dosage and avoid potential interactions with other medications. Vitamin D is equally important, as it facilitates calcium absorption in the gut. Dietary sources include fatty fish, egg yolks, and fortified foods. Sunlight exposure also contributes to vitamin D production in the skin. However, insufficient sunlight exposure or dietary intake often necessitates vitamin D supplementation. A healthcare provider can assess individual needs and recommend the appropriate dosage. Combining adequate calcium and vitamin D intake with other bone-health promoting strategies maximizes the positive effects on bone density during and after tamoxifen treatment.
Physical Activity and Exercise⁚ Building Stronger Bones
Regular physical activity is a cornerstone of maintaining strong bones, especially during tamoxifen therapy. Weight-bearing exercises, which involve working against gravity, are particularly effective in stimulating bone growth and increasing bone density. Examples include walking, jogging, hiking, dancing, and climbing stairs. Resistance training, using weights or resistance bands, further strengthens bones and improves muscle mass, reducing the risk of falls and fractures. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, combined with strength training exercises at least twice a week. Before starting any new exercise program, it’s advisable to consult a healthcare professional or physical therapist to create a safe and effective plan tailored to individual needs and limitations. They can assess any potential risks associated with specific activities, particularly given the possible side effects of tamoxifen. Consistent engagement in a suitable exercise program significantly contributes to optimizing bone health during and after tamoxifen treatment.
Addressing Concerns About Bone Loss⁚ Prevention and Management
Addressing concerns about bone loss during tamoxifen therapy requires a proactive and multi-faceted approach. Prevention is key; maintaining a healthy lifestyle with adequate calcium and vitamin D intake, regular weight-bearing exercise, and avoidance of smoking and excessive alcohol consumption significantly reduces the risk of bone loss. Regular monitoring of bone mineral density (BMD) through bone density scans allows for early detection of any significant bone loss. If BMD testing reveals concerning trends, various management strategies can be implemented. These may include lifestyle modifications, as mentioned above, and supplementation with calcium and vitamin D if dietary intake is insufficient. In more severe cases, pharmacological interventions, such as bisphosphonates or other bone-protective medications, might be considered under the guidance of a healthcare professional. The choice of management strategy depends on individual risk factors, the severity of bone loss, and the patient’s overall health status. A collaborative approach, involving the oncologist and other healthcare providers, ensures the most appropriate and effective management plan.
Pharmacological Interventions⁚ Medications to Protect Bone Health
In some cases, pharmacological interventions may be necessary to address bone loss concerns during tamoxifen therapy. Bisphosphonates, a class of medications commonly used to treat osteoporosis, work by inhibiting bone resorption, the process by which bone is broken down. This can help maintain bone density and reduce the risk of fractures. Other medications, such as teriparatide, a parathyroid hormone analog, can stimulate bone formation. Denosumab, a monoclonal antibody, targets a protein involved in bone resorption, inhibiting its activity and promoting bone growth. The choice of pharmacological intervention depends on individual factors, such as the severity of bone loss, the patient’s overall health status, and other medications being taken. These medications can be effective in preserving bone density and reducing the risk of fractures, but they also have potential side effects, which should be discussed with a healthcare professional. Regular monitoring of bone mineral density and assessment of medication effectiveness are essential to ensure optimal outcomes and minimize potential risks.
The Importance of Regular Health Checkups and Monitoring
Regular health checkups and monitoring are crucial during tamoxifen therapy to assess overall health, track bone health, and proactively address any potential side effects. These checkups typically include a physical exam, blood tests, and a discussion of any symptoms or concerns. Monitoring bone health specifically involves regular bone mineral density (BMD) scans to assess bone density and identify any changes over time. The frequency of BMD scans may vary depending on individual risk factors and the duration of tamoxifen therapy. By closely monitoring bone health, healthcare professionals can detect early signs of bone loss and intervene promptly with appropriate measures, such as lifestyle modifications or pharmacological interventions, to prevent or minimize bone loss. Regular health checkups also provide an opportunity to discuss other aspects of health, such as general well-being, tolerability of tamoxifen therapy, and any other concerns or questions the patient may have.
Comparing Tamoxifen with Other Breast Cancer Treatments⁚ Bone Health Considerations
When considering different breast cancer treatments, understanding their potential impact on bone health is important. Compared to other commonly used breast cancer treatments, such as aromatase inhibitors (AIs) and chemotherapy, tamoxifen has distinct effects on bone density. AIs, such as anastrozole, letrozole, and exemestane, can lead to a decrease in bone mineral density (BMD) due to their mechanism of action, which involves lowering estrogen levels. Chemotherapy regimens, on the other hand, can also have negative effects on bone health, particularly in premenopausal women. In contrast, tamoxifen, while having different effects on bone density in premenopausal and postmenopausal women, generally has a more favorable impact on bone health, especially in postmenopausal women, where it can help maintain or even increase BMD. This is due to its partial estrogen agonist activity on bone receptors. Therefore, when selecting the most appropriate breast cancer treatment, healthcare professionals consider various factors, including the patient’s menopausal status, overall health, and potential impact on bone health, to make personalized treatment decisions.
Aromatase Inhibitors and Bone Density⁚ A Comparison with Tamoxifen
Aromatase inhibitors (AIs), such as anastrozole, letrozole, and exemestane, are commonly used in breast cancer treatment, particularly in postmenopausal women. AIs work by reducing estrogen production, which can lead to a decrease in bone mineral density (BMD). This is because estrogen plays a crucial role in maintaining bone health. In contrast, tamoxifen, another breast cancer treatment, has different effects on bone density. In postmenopausal women, tamoxifen can help maintain or even increase BMD due to its partial estrogen agonist activity on bone receptors. Therefore, when considering the impact on bone health, tamoxifen may be a more favorable option for postmenopausal women compared to AIs. However, it’s important to note that the choice of treatment depends on various factors, including the patient’s menopausal status, overall health, and other individual considerations. Healthcare professionals carefully evaluate these factors and discuss the potential risks and benefits with the patient to determine the most appropriate treatment plan.
Long-Term Effects of Tamoxifen on Bone Density⁚ A Continuing Assessment
Long-term use of tamoxifen in breast cancer treatment raises questions about its sustained effects on bone density. While studies have shown that tamoxifen can help maintain or even increase BMD in postmenopausal women during the initial years of treatment, its long-term impact requires ongoing assessment. Some research suggests that the positive effects on BMD may diminish over time, particularly in women who experience early menopause or have other risk factors for osteoporosis. Therefore, regular monitoring of BMD and lifestyle modifications to promote bone health remain important for women taking tamoxifen long-term. Healthcare professionals continue to investigate the long-term effects of tamoxifen on bone health to provide optimal care and guidance to patients receiving this treatment.
Balancing the Benefits and Risks of Tamoxifen
Tamoxifen’s role in breast cancer treatment involves a careful consideration of its benefits and risks, including its impact on bone density. While tamoxifen can be an effective treatment for breast cancer, particularly in postmenopausal women, its potential effects on bone health must be managed proactively. Regular monitoring of bone mineral density, along with lifestyle modifications to promote bone health, is essential for women taking tamoxifen long-term. Healthcare professionals play a crucial role in educating patients about the potential risks and benefits of tamoxifen and working with them to develop individualized treatment plans that optimize both cancer treatment outcomes and bone health.
Further Research and Ongoing Studies⁚ Future Directions
Ongoing research and clinical studies continue to explore various aspects of tamoxifen’s effects on bone density and overall bone health. These studies aim to refine our understanding of the long-term implications of tamoxifen treatment and identify strategies to mitigate potential risks. Investigating the combined effects of tamoxifen with other breast cancer treatments, such as aromatase inhibitors, on bone health is also an area of active research. Additionally, studies are examining the role of genetic factors, lifestyle interventions, and nutritional approaches in optimizing bone health during and after tamoxifen therapy. The findings from these ongoing studies will contribute to the development of evidence-based guidelines and personalized treatment plans for women receiving tamoxifen, ultimately improving their long-term health outcomes.

