Tamoxifen⁚ A Comprehensive Overview
Tamoxifen, a selective estrogen receptor modulator (SERM), is utilized in breast cancer treatment and prevention. It impedes estrogen’s action in breast tissue, inhibiting tumor growth. This overview explores tamoxifen’s multifaceted role, encompassing its mechanism of action, clinical applications, and potential adverse effects.
Mechanism of Action
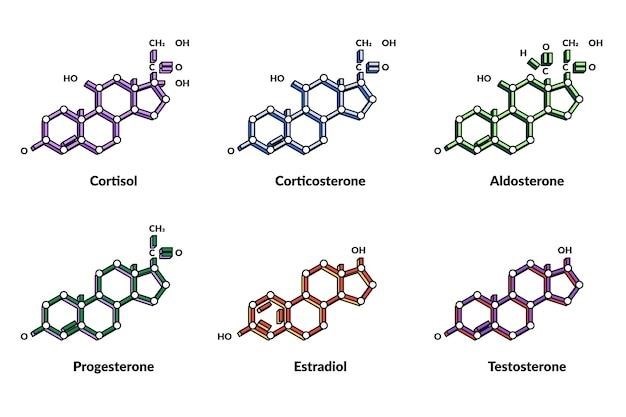
Tamoxifen functions as a selective estrogen receptor modulator (SERM), exhibiting both estrogenic and anti-estrogenic properties depending on the target tissue. Its primary mechanism of action in breast cancer treatment revolves around its competitive binding to estrogen receptors (ERs) within breast cells. By occupying these receptors, tamoxifen effectively blocks estrogen, a hormone that can stimulate the growth of estrogen-receptor-positive breast cancers, from binding and exerting its proliferative effects.
While acting as an antagonist in breast tissue, tamoxifen can display estrogenic effects in other tissues, such as bone and the uterus. This tissue-specific activity stems from the complex interplay between tamoxifen, its metabolites, and the ER subtypes (ERα and ERβ). The binding of tamoxifen to ER alters the receptor’s conformation, influencing its interaction with coactivators and corepressors, ultimately modulating gene transcription. This intricate mechanism accounts for tamoxifen’s efficacy in breast cancer treatment while also contributing to its potential side effects.
Furthermore, tamoxifen’s metabolites, particularly 4-hydroxytamoxifen and endoxifen, play a significant role in its overall activity. Endoxifen, a potent anti-estrogen, contributes substantially to tamoxifen’s therapeutic effects. Variations in the metabolism of tamoxifen, influenced by genetic factors like CYP2D6 polymorphisms, can affect the concentration of active metabolites and consequently impact treatment response.
Approved Indications and Usage
Tamoxifen holds several key approvals for breast cancer management. It is indicated for the treatment of metastatic breast cancer in both premenopausal and postmenopausal women and men. This includes patients with hormone receptor-positive (estrogen receptor (ER) and/or progesterone receptor (PR) positive) and hormone receptor-unknown metastatic breast cancer. For patients with ER-positive metastatic disease, tamoxifen is particularly effective.
In the adjuvant setting, tamoxifen is approved for use after surgery and radiation therapy in women with node-positive or node-negative breast cancer. This adjuvant therapy aims to reduce the risk of recurrence and improve overall survival. Furthermore, tamoxifen is indicated for the reduction of breast cancer incidence in high-risk women. This chemoprevention strategy targets women with ductal carcinoma in situ (DCIS) and those identified as high-risk based on established risk assessment models.
Importantly, the efficacy of tamoxifen is most pronounced in patients with estrogen receptor-positive tumors. The presence of ER positivity signifies that the tumor’s growth is fueled by estrogen, making it susceptible to tamoxifen’s anti-estrogenic effects. While tamoxifen can be used in patients with hormone receptor-unknown status, its benefits are more predictable and substantial in the ER-positive population.
Treatment of Metastatic Breast Cancer
Tamoxifen plays a crucial role in managing metastatic breast cancer, particularly in patients with hormone receptor-positive disease. In this setting, tamoxifen aims to slow or halt cancer progression by blocking the effects of estrogen on tumor cells. It is utilized in both premenopausal and postmenopausal women, as well as in men with metastatic breast cancer.
For patients with estrogen receptor-positive metastatic breast cancer, tamoxifen is often a first-line endocrine therapy option. Its effectiveness stems from its ability to compete with estrogen for binding to estrogen receptors within tumor cells. This competitive inhibition reduces estrogen-driven tumor growth and can lead to tumor regression or stabilization. The duration of treatment for metastatic disease is generally indefinite, continuing as long as the patient benefits and tolerates the therapy.
While tamoxifen’s efficacy is most pronounced in ER-positive disease, it can also be considered in patients with hormone receptor-unknown metastatic breast cancer, especially if other treatment options are limited. In these cases, the response to tamoxifen can be less predictable. The choice between tamoxifen and other endocrine therapies, such as aromatase inhibitors, depends on factors including menopausal status, disease characteristics, and patient-specific considerations.
Adjuvant Therapy After Surgery and Radiation
Tamoxifen is a cornerstone of adjuvant therapy for breast cancer, administered following surgery and/or radiation therapy to reduce the risk of recurrence and improve long-term survival. Its role in this setting is primarily for patients with hormone receptor-positive breast cancer, where the presence of estrogen receptors signifies a susceptibility to estrogen-driven tumor growth.
Adjuvant tamoxifen therapy typically spans five years, although longer durations may be considered in certain cases. By blocking estrogen’s action in residual breast tissue, tamoxifen aims to eradicate micrometastatic disease and prevent the emergence of recurrent tumors. This proactive approach substantially improves disease-free survival and overall survival rates in patients with hormone-responsive breast cancer.
The decision to utilize tamoxifen as adjuvant therapy considers factors such as the patient’s menopausal status, tumor characteristics (including hormone receptor status and tumor size), lymph node involvement, and individual risk factors. For premenopausal women, tamoxifen is often the preferred adjuvant endocrine therapy. In postmenopausal women, the choice between tamoxifen and aromatase inhibitors may depend on individual patient characteristics and risk assessment.
Risk Reduction in High-Risk Patients
Tamoxifen plays a significant role in breast cancer risk reduction for women identified as high-risk based on established risk assessment models. These models incorporate factors such as age, family history of breast cancer, reproductive history, and breast biopsy findings to estimate an individual’s likelihood of developing the disease. For women deemed high-risk, tamoxifen offers a chemoprevention strategy to reduce the incidence of invasive breast cancer.
Clinical trials have demonstrated that tamoxifen can significantly lower the risk of developing invasive breast cancer in high-risk women. The duration of chemoprevention therapy is typically five years. While tamoxifen can be effective in reducing risk, it’s essential to carefully weigh the potential benefits against the possible side effects. A thorough discussion with a healthcare professional is crucial to make an informed decision.
The decision to initiate tamoxifen for risk reduction considers the individual’s risk profile, potential benefits, and potential adverse effects. Factors such as age, overall health status, and the presence of risk factors for specific side effects (e.g., thromboembolic events) are carefully evaluated. Shared decision-making between the patient and healthcare provider is paramount in determining the appropriateness of tamoxifen for chemoprevention.
Estrogen Receptor-Positive Tumors
Tamoxifen’s efficacy is intrinsically linked to the presence of estrogen receptors (ERs) in breast tumor cells. ER-positive tumors rely on estrogen to fuel their growth and proliferation. Tamoxifen acts as an antagonist in these tumors, effectively blocking estrogen from binding to its receptors and thereby inhibiting estrogen-driven tumor growth. This targeted mechanism of action makes tamoxifen particularly effective in treating and preventing ER-positive breast cancer.
The determination of ER status is a crucial step in breast cancer diagnosis and treatment planning. ER positivity, determined through laboratory testing of tumor tissue, predicts a higher likelihood of response to endocrine therapies like tamoxifen. Conversely, ER-negative tumors lack these receptors and are less likely to benefit from tamoxifen treatment. Other therapeutic approaches, such as chemotherapy or targeted therapies, are typically employed for ER-negative breast cancer.
The degree of ER positivity can also influence treatment decisions. Tumors with higher levels of ER expression tend to exhibit a greater response to tamoxifen compared to those with lower ER expression. This information, along with other clinical and pathological factors, guides the selection of the most appropriate treatment strategy for individual patients with ER-positive breast cancer.
Pharmacokinetics and Metabolism
Tamoxifen undergoes extensive metabolism in the liver, primarily through the cytochrome P450 (CYP) enzyme system, specifically CYP2D6. This metabolic process transforms tamoxifen into several active metabolites, including 4-hydroxytamoxifen and endoxifen, which contribute significantly to its therapeutic effects. Endoxifen, in particular, exhibits a substantially higher affinity for estrogen receptors compared to tamoxifen itself.
Following oral administration, tamoxifen is well-absorbed, reaching peak plasma concentrations within several hours. It is highly lipophilic and distributes widely throughout the body, accumulating in fatty tissues. Tamoxifen has a long elimination half-life, typically ranging from 5 to 7 days, leading to sustained drug levels in the body. This prolonged half-life allows for once-daily dosing.
The extensive hepatic metabolism and enterohepatic recirculation of tamoxifen contribute to its complex pharmacokinetic profile. Genetic variations in CYP2D6 activity can influence the formation of active metabolites and consequently affect treatment response. Patients with reduced CYP2D6 activity may experience lower levels of endoxifen, potentially impacting tamoxifen’s efficacy. Therapeutic drug monitoring and consideration of alternative endocrine therapies may be warranted in these cases.
CYP2D6 Metabolism and Implications
The metabolism of tamoxifen is heavily reliant on the cytochrome P450 2D6 (CYP2D6) enzyme. This enzyme converts tamoxifen into its active metabolites, including endoxifen, which possesses significantly greater anti-estrogenic potency than the parent drug; Variations in CYP2D6 activity, influenced by genetic polymorphisms, can significantly impact the efficacy of tamoxifen therapy.
Patients with certain CYP2D6 genotypes, categorized as poor metabolizers, exhibit reduced enzyme activity and consequently produce lower levels of endoxifen. This diminished endoxifen concentration can lead to suboptimal therapeutic outcomes and potentially increase the risk of breast cancer recurrence. Conversely, patients with normal or increased CYP2D6 activity achieve higher endoxifen levels and are more likely to experience the full benefits of tamoxifen therapy.
The clinical implications of CYP2D6 genotype necessitate careful consideration in treatment planning. Genotyping may be performed to assess CYP2D6 activity and guide treatment decisions. For patients identified as poor metabolizers, alternative endocrine therapies, such as aromatase inhibitors, may be considered to ensure optimal disease control. Therapeutic drug monitoring can also be employed to assess endoxifen levels and adjust tamoxifen dosage as needed.
Dosage and Administration
Tamoxifen is administered orally, typically as a tablet, once daily. The standard dosage for the treatment of breast cancer is 20 mg per day. However, dosages may be adjusted based on individual patient factors, such as tolerability and concomitant medications. The duration of therapy varies depending on the specific indication. For adjuvant treatment following surgery or radiation therapy, the recommended duration is typically five years. In the setting of metastatic breast cancer, treatment may continue indefinitely as long as the patient derives benefit and tolerates the medication.
For risk reduction in high-risk women, the standard dosage is also 20 mg per day, administered for five years. It’s crucial to adhere to the prescribed dosage and duration of therapy to maximize the benefits of tamoxifen treatment. Patients should be instructed to take tamoxifen consistently, preferably at the same time each day, with or without food. Missed doses should be taken as soon as remembered, unless it is close to the time of the next scheduled dose. Double dosing should be avoided.
Regular follow-up with a healthcare provider is essential during tamoxifen therapy to monitor treatment response, manage potential side effects, and address any patient concerns. Dosage adjustments may be necessary based on individual patient response and tolerability. Open communication between the patient and healthcare provider is crucial for optimizing tamoxifen therapy and ensuring its safe and effective use.
Duration of Therapy
The optimal duration of tamoxifen therapy depends on the specific clinical context, encompassing the indication for treatment and individual patient factors. In the adjuvant setting, following surgery or radiation therapy for early-stage breast cancer, the standard recommendation is five years of tamoxifen treatment. This extended duration aims to suppress residual microscopic disease and reduce the risk of recurrence.
For women at high risk of developing breast cancer, tamoxifen is also typically prescribed for five years as a chemopreventive measure. This strategy aims to reduce the incidence of invasive breast cancer by modulating estrogen’s effects on breast tissue. In the case of metastatic breast cancer, tamoxifen therapy is often continued indefinitely as long as the patient demonstrates clinical benefit and tolerates the treatment. The goal in this setting is to control disease progression and improve overall survival.
The decision regarding the duration of tamoxifen therapy involves a careful assessment of individual patient characteristics, including age, menopausal status, tumor characteristics, and the presence of comorbidities. Ongoing monitoring of treatment response and potential side effects is essential throughout the course of therapy. Shared decision-making between the patient and healthcare provider is crucial to determine the most appropriate duration of treatment based on individual circumstances and clinical goals.
Adverse Effects and Side Effects
Tamoxifen therapy, while generally well-tolerated, can be associated with a range of adverse effects, varying in severity and frequency. Common side effects include hot flashes, vaginal dryness, irregular menstrual periods (in premenopausal women), and mild nausea. These effects are often manageable and do not necessitate discontinuation of therapy.
More serious, albeit less frequent, side effects include an increased risk of endometrial cancer, thromboembolic events (such as deep vein thrombosis and pulmonary embolism), and stroke. Regular monitoring and prompt evaluation of any concerning symptoms are crucial. The risk-benefit profile of tamoxifen should be carefully considered, particularly in patients with pre-existing risk factors for these serious adverse events.
Ocular side effects, such as cataracts and retinopathy, can also occur, though they are less common. Regular ophthalmological examinations are recommended for patients on long-term tamoxifen therapy. Additionally, some patients may experience mood changes, fatigue, or alterations in bone density. A comprehensive understanding of the potential adverse effects is essential for informed decision-making and appropriate management of any emergent issues during tamoxifen treatment.
Common Side Effects (Hot Flashes, Nausea, etc.)
Tamoxifen therapy frequently elicits relatively mild side effects that, while often bothersome, are generally manageable and rarely necessitate treatment discontinuation. Hot flashes, characterized by a sudden sensation of warmth in the upper body, are a common occurrence. Vaginal dryness, often accompanied by discomfort or itching, is another frequently reported side effect. In premenopausal women, tamoxifen can disrupt menstrual cycles, leading to irregular periods or amenorrhea.
Nausea, though typically mild, can occur in some patients. Other common side effects include weight fluctuations, mild hair thinning, and skin changes, such as dryness or rash. These effects are typically transient and subside over time. Management strategies for these common side effects include lifestyle modifications, such as maintaining a comfortable temperature, using vaginal lubricants, and adopting stress-reduction techniques.
Open communication with healthcare providers is crucial for addressing these common side effects and exploring appropriate management strategies. Patients should be reassured that these effects are often temporary and manageable. In some cases, symptomatic relief can be achieved through pharmacological interventions or complementary therapies. The decision to implement such interventions should be individualized based on the severity of symptoms and patient preferences.
Serious Side Effects (Uterine Cancer, Blood Clots, etc.)
While tamoxifen offers significant benefits in breast cancer treatment and prevention, it carries a risk of serious side effects that warrant careful monitoring and proactive management. One notable concern is the increased risk of endometrial cancer in women taking tamoxifen. Regular gynecological examinations and prompt evaluation of any abnormal vaginal bleeding are crucial for early detection and intervention.
Tamoxifen can also increase the risk of thromboembolic events, including deep vein thrombosis (DVT) and pulmonary embolism (PE). These events occur when blood clots form in the deep veins, potentially traveling to the lungs and causing life-threatening complications. Patients should be educated about the signs and symptoms of DVT and PE, such as leg pain, swelling, and shortness of breath, and seek immediate medical attention if these occur. Additionally, tamoxifen carries a slightly increased risk of stroke, particularly in women with pre-existing risk factors.
While these serious side effects are less common than the milder side effects, their potential severity necessitates careful consideration. The decision to initiate tamoxifen therapy involves a thorough assessment of the individual’s risk-benefit profile. Regular monitoring and prompt management of any emergent serious side effects are essential to ensure patient safety and optimize treatment outcomes.
Endometrial Effects and Monitoring
Tamoxifen’s estrogenic effects on the endometrium, the lining of the uterus, represent a significant consideration in its use. While tamoxifen primarily acts as an anti-estrogen in breast tissue, it can stimulate endometrial growth in some women. This stimulation increases the risk of endometrial hyperplasia, a thickening of the endometrial lining, which can progress to endometrial cancer if left unmanaged.
Regular monitoring of the endometrium is therefore essential for women undergoing tamoxifen therapy. Transvaginal ultrasound is often employed to assess endometrial thickness. Any significant increase in endometrial thickness or the detection of abnormal findings necessitates further evaluation and potential intervention. Endometrial biopsies may be performed to rule out hyperplasia or cancer;
The frequency of endometrial monitoring depends on several factors, including the patient’s age, risk profile, and the presence of any concerning symptoms. Generally, monitoring is recommended at baseline before starting tamoxifen and periodically throughout the course of treatment. Prompt attention to any abnormal vaginal bleeding, which could indicate endometrial pathology, is paramount. Close collaboration between the patient and healthcare provider is crucial for effective monitoring and management of endometrial effects associated with tamoxifen therapy.
Cardiovascular Risks
The use of tamoxifen is associated with a modest increase in the risk of cardiovascular events, although the magnitude of this risk remains a subject of ongoing investigation and debate within the medical community. Studies have shown a slightly elevated risk of thromboembolic events, such as deep vein thrombosis (DVT) and pulmonary embolism (PE), in patients receiving tamoxifen compared to those not receiving the medication.
The increased risk of thromboembolic events is thought to be related to tamoxifen’s effects on blood clotting factors. Patients with pre-existing cardiovascular risk factors, such as a history of DVT or PE, hypertension, or smoking, may be at particularly increased risk. Careful assessment of cardiovascular risk factors is therefore essential before initiating tamoxifen therapy.
Patients should be educated about the signs and symptoms of DVT and PE, and prompt medical attention should be sought if these occur. Lifestyle modifications, such as maintaining adequate hydration, avoiding prolonged periods of immobility, and cessation of smoking, can help mitigate the risk. In patients with significant cardiovascular risk factors, the benefits of tamoxifen therapy should be carefully weighed against the potential cardiovascular risks. Alternative endocrine therapies may be considered in certain cases.
Contraindications and Precautions
Several contraindications and precautions are associated with tamoxifen use, necessitating careful patient selection and ongoing monitoring. A primary contraindication is pregnancy. Tamoxifen is categorized as a pregnancy category D medication, indicating a positive evidence of risk to the fetus. Therefore, women of childbearing potential must employ effective contraception during tamoxifen therapy and for at least two months following treatment cessation.
Pre-existing thromboembolic disorders represent another significant contraindication. Patients with a history of DVT, PE, or stroke should generally not receive tamoxifen due to the increased risk of recurrent events. Caution is also warranted in patients with a history of liver disease, as tamoxifen is extensively metabolized in the liver. Close monitoring of liver function is recommended.
Patients with a history of uterine bleeding of unknown etiology or those with known endometrial hyperplasia or cancer should also avoid tamoxifen. In patients with pre-existing conditions or risk factors for serious adverse events, the potential benefits of tamoxifen therapy must be carefully weighed against the risks. A thorough discussion with a healthcare provider is crucial to determine the appropriateness of tamoxifen in these situations.
Pregnancy and Lactation
Tamoxifen is contraindicated during pregnancy due to its potential teratogenic effects. Studies have demonstrated an increased risk of fetal abnormalities and adverse pregnancy outcomes in women exposed to tamoxifen during gestation. Therefore, effective contraception is mandatory for women of childbearing potential throughout the duration of tamoxifen therapy and for at least two months after treatment completion.
The decision to use tamoxifen in breastfeeding women requires careful consideration. Tamoxifen is excreted in breast milk, and its potential effects on the nursing infant are not fully understood. The risk-benefit ratio should be carefully evaluated, weighing the potential benefits of tamoxifen for the mother against the potential risks to the infant. In some cases, discontinuation of breastfeeding may be recommended during tamoxifen therapy.
Healthcare providers should counsel patients regarding the risks associated with tamoxifen use during pregnancy and lactation. Women should be strongly advised to avoid becoming pregnant while taking tamoxifen and to utilize effective contraceptive methods. Individualized risk-benefit assessments are crucial for guiding treatment decisions in women who are pregnant, planning to become pregnant, or breastfeeding.
Drug Interactions
Tamoxifen’s metabolism and pharmacodynamic effects can be influenced by concomitant medications, necessitating careful consideration of potential drug interactions. Drugs that inhibit CYP2D6, the enzyme primarily responsible for tamoxifen metabolism, can reduce the formation of active metabolites, potentially compromising its efficacy. Examples of CYP2D6 inhibitors include selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine and paroxetine, and some antiarrhythmic drugs.
Conversely, drugs that induce CYP2D6 activity can accelerate tamoxifen metabolism, potentially reducing its therapeutic effect. Such inducers include rifampin, a common antibiotic, and St. John’s wort, an herbal supplement. The use of these medications concurrently with tamoxifen requires careful monitoring and potential dosage adjustments. Clinicians should assess the patient’s medication history to identify potential drug interactions.
The interaction potential of tamoxifen extends beyond CYP2D6. Concurrent use with certain anticoagulants, such as warfarin, may enhance the risk of bleeding. Similarly, concurrent use with certain chemotherapy agents may alter the pharmacokinetics or pharmacodynamics of either drug. A thorough review of the patient’s medication regimen, including prescription medications, over-the-counter drugs, and herbal supplements, is essential to minimize the likelihood of clinically significant drug interactions.
Tamoxifen Resistance
Despite its initial effectiveness, some breast cancers eventually develop resistance to tamoxifen, necessitating alternative therapeutic strategies. This resistance can manifest as either primary resistance, where the tumor fails to respond to tamoxifen from the outset, or acquired resistance, where an initial response is followed by disease progression.
The mechanisms underlying tamoxifen resistance are complex and multifactorial. Alterations in estrogen receptor (ER) function, including mutations or reduced ER expression, can impair tamoxifen’s ability to bind and inhibit ER signaling. Changes in downstream signaling pathways, independent of ER, can also contribute to resistance. Furthermore, alterations in the expression of other genes involved in cell growth and proliferation can bypass the inhibitory effects of tamoxifen.
Understanding the mechanisms of tamoxifen resistance is crucial for developing effective strategies to overcome it. Research is ongoing to identify biomarkers predictive of resistance and to develop novel therapeutic approaches that target these resistance mechanisms. This includes the investigation of novel agents that can restore sensitivity to tamoxifen or circumvent resistance pathways altogether. A personalized approach to treatment, tailored to the specific mechanisms of resistance in individual patients, is essential for optimizing long-term outcomes.
Mechanisms of Resistance
The development of resistance to tamoxifen in breast cancer is a complex process involving multiple interconnected mechanisms. One key mechanism is alterations in the estrogen receptor (ER) itself. Mutations in the ER gene can affect the receptor’s ability to bind tamoxifen, reducing its inhibitory effects. Furthermore, reduced ER expression, where fewer ERs are present on the surface of tumor cells, can also contribute to resistance.
Beyond alterations in the ER, other intracellular signaling pathways can mediate tamoxifen resistance. Activation of growth factor receptor signaling pathways, such as the epidermal growth factor receptor (EGFR) pathway, can bypass the inhibitory effects of tamoxifen on ER signaling. Changes in the expression of genes involved in cell cycle regulation and apoptosis can also contribute to resistance, allowing tumor cells to proliferate unchecked despite tamoxifen’s presence.
Furthermore, the tumor microenvironment plays a crucial role in mediating tamoxifen resistance. Factors such as increased expression of growth factors and cytokines within the tumor microenvironment can stimulate tumor growth and promote resistance; The interplay of these various mechanisms highlights the complexity of tamoxifen resistance and underscores the need for a multifaceted approach to overcome it. This necessitates the development of novel therapeutic strategies targeting multiple pathways simultaneously.
Overcoming Resistance
Overcoming tamoxifen resistance in breast cancer requires a multifaceted approach, often involving a shift in therapeutic strategies. One approach involves switching to alternative endocrine therapies, such as aromatase inhibitors, which target a different point in the estrogen synthesis pathway. These agents can be effective even in tumors that have developed resistance to tamoxifen.
The addition of other targeted therapies can also be beneficial. For instance, if resistance is mediated by activation of growth factor receptor pathways, such as the EGFR pathway, targeting these pathways with specific inhibitors can restore sensitivity to tamoxifen or provide additional anti-tumor activity. Similarly, targeting other signaling pathways involved in cell growth and proliferation may prove effective.
Furthermore, combination therapies that utilize multiple agents with different mechanisms of action can be employed. This approach aims to overcome resistance by targeting multiple pathways simultaneously. Research into novel agents that directly target mechanisms of tamoxifen resistance is ongoing, holding promise for the future development of more effective treatment strategies. The selection of optimal strategies for overcoming tamoxifen resistance necessitates careful consideration of individual patient characteristics and the specific mechanisms of resistance driving the disease progression.
Combination Therapies
Combination therapies represent a powerful strategy in managing breast cancer, particularly in overcoming resistance to tamoxifen. Combining tamoxifen with other agents that target different mechanisms of tumor growth can enhance efficacy and improve outcomes. One common combination involves pairing tamoxifen with chemotherapy, particularly in the adjuvant setting, to maximize the destruction of cancer cells and reduce recurrence risk.
The combination of tamoxifen with other endocrine therapies, such as aromatase inhibitors, can also prove beneficial. This approach is particularly relevant in postmenopausal women, where aromatase inhibitors effectively suppress estrogen production, complementing tamoxifen’s action on estrogen receptors. Such combined endocrine therapy can provide superior disease control and improved survival compared to tamoxifen monotherapy.
Furthermore, targeted therapies can be incorporated into combination regimens. For example, combining tamoxifen with agents that inhibit growth factor signaling pathways, such as EGFR inhibitors, may enhance efficacy in tumors that exhibit activation of these pathways. The selection of optimal combination therapies depends on several factors, including the patient’s age, menopausal status, tumor characteristics (hormone receptor status, HER2 status), and overall health. Careful consideration of potential drug interactions and side effects is essential when employing combination therapies.
Clinical Trials and Research
Extensive clinical trials have shaped our understanding of tamoxifen’s efficacy and safety profile in various breast cancer settings. Landmark trials have demonstrated the drug’s effectiveness in reducing breast cancer recurrence in the adjuvant setting and its ability to reduce the incidence of invasive breast cancer in high-risk women. These trials have established tamoxifen as a foundational treatment modality in breast cancer management.
Ongoing research continues to explore the optimal duration of tamoxifen therapy, the identification of predictive biomarkers for treatment response, and the development of strategies to overcome tamoxifen resistance. Studies are investigating the role of genetic factors, such as CYP2D6 polymorphisms, in influencing tamoxifen metabolism and treatment outcomes. Furthermore, research is focused on identifying novel combinations of tamoxifen with other agents to enhance efficacy and reduce resistance.
Clinical trials also investigate the potential benefits of tamoxifen in other cancers and conditions. Research is exploring tamoxifen’s potential role in the prevention and treatment of other hormone-dependent cancers, as well as its potential applications in non-cancer conditions. These ongoing clinical trials and research efforts are crucial for refining our understanding of tamoxifen’s mechanism of action, optimizing treatment strategies, and improving patient outcomes.
Current Research Directions
Current research on tamoxifen focuses on several key areas to enhance its therapeutic efficacy and address limitations. One major focus is overcoming tamoxifen resistance. Researchers are actively investigating the molecular mechanisms underlying resistance, aiming to identify novel therapeutic targets and develop agents that can restore sensitivity to tamoxifen or circumvent resistance pathways.
Another area of intense investigation involves optimizing tamoxifen’s use in specific patient populations. Studies are exploring the role of pharmacogenomics in predicting treatment response and tailoring therapy based on individual genetic profiles. This personalized medicine approach aims to maximize benefits while minimizing adverse effects. Research is also exploring the potential of combining tamoxifen with other targeted therapies to enhance its effectiveness.
Furthermore, research is evaluating the long-term effects of tamoxifen therapy, including its impact on cardiovascular health, bone density, and other organ systems. This long-term surveillance is crucial for understanding the overall risk-benefit profile of tamoxifen and for developing strategies to mitigate potential adverse effects. These ongoing research endeavors aim to refine tamoxifen’s clinical application and improve outcomes for patients with breast cancer.
Future Perspectives
The future of tamoxifen in breast cancer management holds exciting possibilities driven by ongoing research and technological advancements. Personalized medicine approaches, guided by genomic profiling and pharmacogenomics, promise to optimize treatment selection and improve outcomes by tailoring therapy to individual patient characteristics. This includes identifying patients most likely to benefit from tamoxifen and those who might be better served by alternative therapies.
The development of novel agents that overcome tamoxifen resistance is a key area of focus. Researchers are actively exploring mechanisms of resistance and developing targeted therapies to circumvent these pathways. This may involve the identification of new drug targets and the development of agents that can either restore sensitivity to tamoxifen or provide alternative anti-tumor effects in resistant tumors.
Furthermore, the integration of advanced imaging techniques and biomarkers may refine monitoring strategies and improve early detection of treatment failure. This enables timely intervention and a shift to alternative therapies, preventing disease progression. These advancements, combined with a deeper understanding of tamoxifen’s mechanism of action, hold significant promise for improving the efficacy and safety of tamoxifen therapy in the years to come, ultimately enhancing patient outcomes.
Patient Counseling and Education
Comprehensive patient counseling and education are paramount to ensure the safe and effective use of tamoxifen. Patients should receive detailed information regarding the drug’s mechanism of action, its intended benefits, potential side effects, and the importance of adherence to the prescribed regimen. This includes a clear explanation of the purpose of tamoxifen therapy, whether it is for treatment or prevention of breast cancer.
Patients should be educated about common side effects, such as hot flashes, vaginal dryness, and nausea, and provided with strategies for managing these symptoms. This may involve lifestyle modifications, such as maintaining a comfortable temperature, using vaginal lubricants, and adopting stress-reduction techniques. Pharmacological interventions may also be considered for symptom relief. Crucially, patients should understand the signs and symptoms of serious adverse events, including thromboembolic events and abnormal vaginal bleeding.
Patients should be explicitly instructed to report any concerning symptoms to their healthcare provider immediately. Regular follow-up appointments are essential for monitoring treatment response, managing side effects, and addressing any patient concerns. Empowering patients with knowledge and fostering open communication between patients and their healthcare providers are vital for optimizing tamoxifen therapy and ensuring patient safety and well-being.
Importance of Adherence
Adherence to the prescribed tamoxifen regimen is of paramount importance for achieving optimal therapeutic outcomes. Consistent daily intake of the medication, as directed by the healthcare provider, is crucial for maintaining effective drug levels and maximizing the drug’s anti-tumor effects. Interruptions or inconsistencies in medication intake can significantly compromise the efficacy of tamoxifen therapy, increasing the risk of disease recurrence or progression.
Several factors can influence adherence to tamoxifen therapy. Side effects, such as hot flashes, vaginal dryness, and nausea, can be distressing and may lead to medication discontinuation. Patient education and support are essential to address these concerns and develop effective strategies for managing side effects. Furthermore, forgetfulness or lack of understanding regarding the importance of consistent medication intake can contribute to poor adherence.
Strategies to enhance adherence include regular follow-up appointments with healthcare providers, medication reminders, and support groups. Collaborative goal-setting between the patient and healthcare provider can improve adherence by focusing on realistic expectations and strategies for overcoming potential barriers. Consistent monitoring of adherence, coupled with proactive patient education and support, is crucial for ensuring that patients receive the full benefits of tamoxifen therapy.
Managing Side Effects
Effective management of tamoxifen’s side effects is crucial for optimizing treatment adherence and improving patient quality of life. Many common side effects, such as hot flashes, can be managed through lifestyle modifications. These include maintaining a cool environment, dressing in layers, avoiding spicy foods and alcohol, and practicing stress-reduction techniques like yoga or meditation. Over-the-counter medications, such as acetaminophen, can be used to manage mild discomfort.
Vaginal dryness can be alleviated with the use of vaginal lubricants or moisturizers. For menstrual irregularities, patients should be counseled on expected changes and provided strategies for managing any associated discomfort. In cases of more severe or persistent side effects, pharmacological interventions may be necessary. For example, selective serotonin reuptake inhibitors (SSRIs) can be effective in managing hot flashes, while hormone replacement therapy may be considered for menopausal symptoms.
Regular monitoring by healthcare providers is essential for identifying and managing potential side effects; Patients should be encouraged to report any new or worsening symptoms promptly. A collaborative approach, involving open communication between patients and their healthcare teams, is key to developing individualized management plans that address the specific needs and concerns of each patient, ensuring optimal tolerability and adherence to tamoxifen therapy.

